Background introduction
IgE is one of the five major immunoglobulins in the body (IgA, IgM, IgG, IgD, and IgE) and is produced by B lymphocytes. It was first recognized in 1967 as an antibody associated with allergic reactions. The structure of the IgE molecule differs from other immunoglobulins in that it has four subunits instead of the common structure of two heavy chains and two light chains. This unique structure allows IgE to bind efficiently to FcεRI receptors on the surface of mast cells and eosinophils.

When the body is exposed to allergens, the immune system recognizes these foreign substances and produces specific IgE antibodies. These IgE antibodies then attach to the surface of mast cells and eosinophils, sensitizing these cells to the allergen. If the allergen re-enters the body, it will bind to IgE antibodies that are already attached to the surface of cells, triggering these cells to release histamine and other inflammatory mediators, leading to typical allergy symptoms such as sneezing, runny nose, red skin and itching.
IgE production
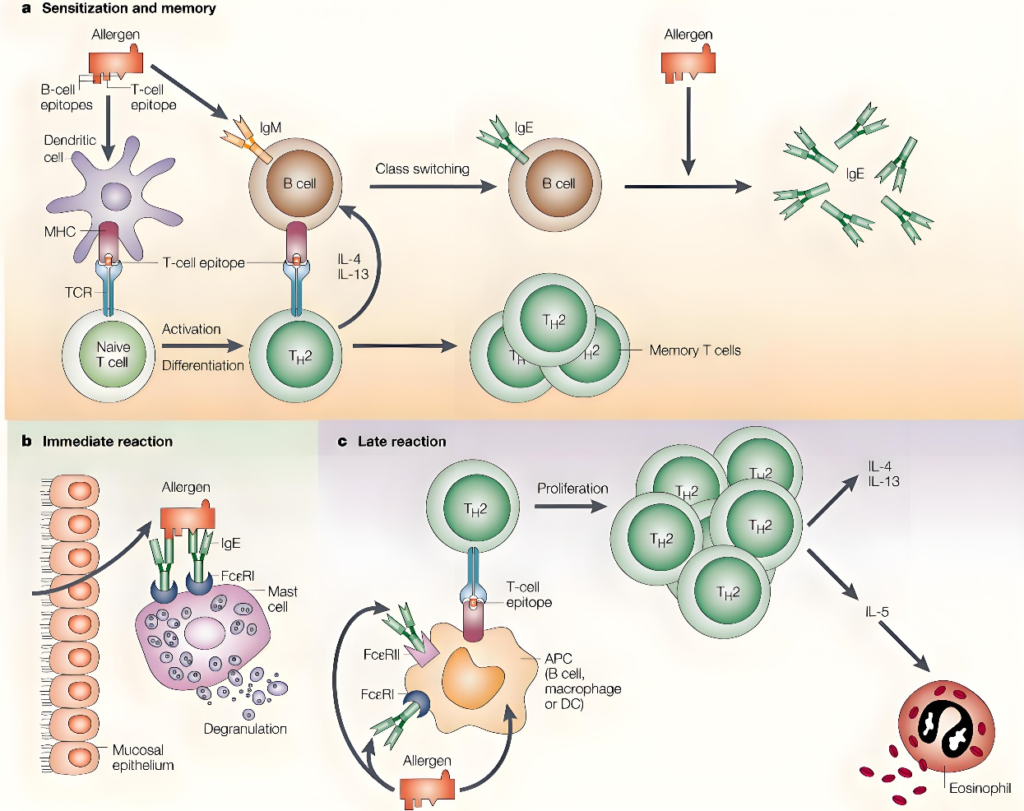
Immunoglobulin E (IgE) production is a complex and finely regulated process involving multiple cell types and molecular signaling pathways in the immune system. When the body encounters a specific antigen (such as a parasite or an allergen), the antigen is captured by antigen-presenting cells (such as dendritic cells) and processed into antigenic peptides, which are then presented to T cells in conjunction with major histocompatibility complex (MHC) molecules. Specific types of T cells, mainly Th2 cells, are activated upon recognition of antigenic peptide-MHC complexes. Activated Th2 cells secrete a series of cytokines, such as interleukin-4 (IL-4), IL-5, IL-13, etc., which are essential for the differentiation and IgE production of B cells. Cytokines secreted by Th2 cells, especially IL-4, stimulate B cells to activate from the naive state and begin to differentiate. In this process, B cells, which receive antigen-specific signals and Th2 cytokines, undergo a process called “class switching” from B cells that produce IgM to B cells that can synthesize IgE. Class-switched B cells begin to synthesize IgE antibodies in large quantities.
Function of IgE
Immunoglobulin E (IgE), as a special antibody in the immune system, has complex biological characteristics. It not only protects the body from parasites, but also may trigger allergic reactions, showing the dual role of the immune system in maintaining the health of the body, highlighting the importance of the immune system to maintain a delicate balance.
Protective Role: Against Parasites IgE plays a vital role in the host’s defense against parasitic infections, especially helminth infections. When parasites enter the human body, IgE can quickly recognize and bind these foreign invaders, release a series of inflammatory mediators, such as histamine and leukotrienes, by activating mast cells and basophils, and then trigger local inflammatory response, effectively preventing further invasion and reproduction of parasites. This mechanism reflects the function of IgE as the first line of defense of the immune system, ensuring that the body can respond to and eliminate threats in a timely manner.
Triggering Allergy: The protective mechanisms of IgE may be out of balance in some cases, resulting in an overreaction to a harmless substance, known as anaphylaxis. When the body is first exposed to a specific allergen, such as pollen, dust mites, or certain food ingredients, the immune system may mistakenly recognize it as a threat, prompting B lymphocytes to produce specific IgE antibodies in large numbers. These IgE antibodies then attach to the surface of mast cells and basophils, forming a “pre-sensitized” state. Upon re-exposure to the same allergen, IgE binds to the allergen, triggering the activation and degranulation of mast cells and basophils, releasing a large number of inflammatory mediators, leading to the appearance of allergic symptoms.
Overall, the allergen IgE is a complex player in the immune system that plays a central role in allergic reactions and is also involved in the body’s defense mechanisms. Understanding the function of IgE and its role in allergy is critical to the development of effective treatment strategies.
Detection of serum total IgE and its clinical significance
1. Serum total IgE detection method
The detection methods of serum total IgE mainly include radioallergosorbent test (radio allergo sorbent test, RAST), enzyme-linked immunosorbent assay (ELISA, enzyme linked immunosorbent assay), ELISA), indirect hemagglutination test and chemiluminescence method. The detection of total IgE is mainly to determine the level of total IgE in human serum or plasma, while the content of IgE in normal human serum is relatively small, usually in the range of 0.1-0.9 mg/L.

2. Clinical significance of serum total IgE
Screening and diagnosis of allergic diseases: The increase of serum total IgE level can indicate that the individual may have allergic constitution or allergic diseases, such as allergic asthma, allergic rhinitis, atopic dermatitis, urticaria, etc.
– Monitoring the effect of treatment of allergic diseases: During the treatment of allergic diseases, such as immunotherapy (desensitization therapy), monitoring the change of total serum IgE level can evaluate the effect of treatment and disease control.
– Auxiliary Diagnosis of Parasitic Infections: Elevated levels of total IgE can also be seen in certain parasitic infections, such as helminth infections. In addition to allergic diseases, the detection of total IgE can help identify the presence of parasitic infections.
Evaluation of immune function: Abnormally high or low levels of total IgE may indicate abnormalities in the immune system, such as immunodeficiency diseases or certain immune-mediated diseases.
Product recommendation
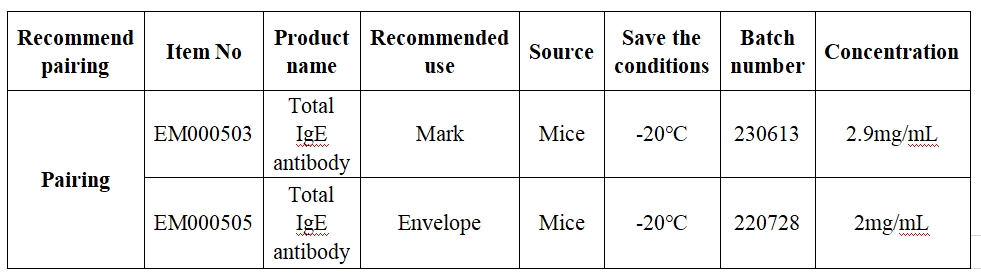
1. Total IgE Recommended Matched Material
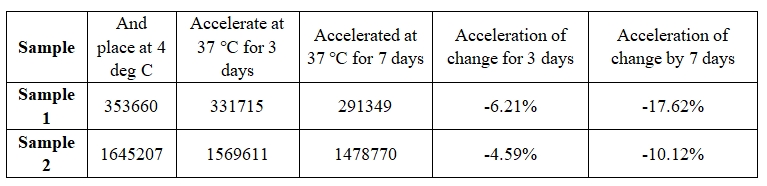
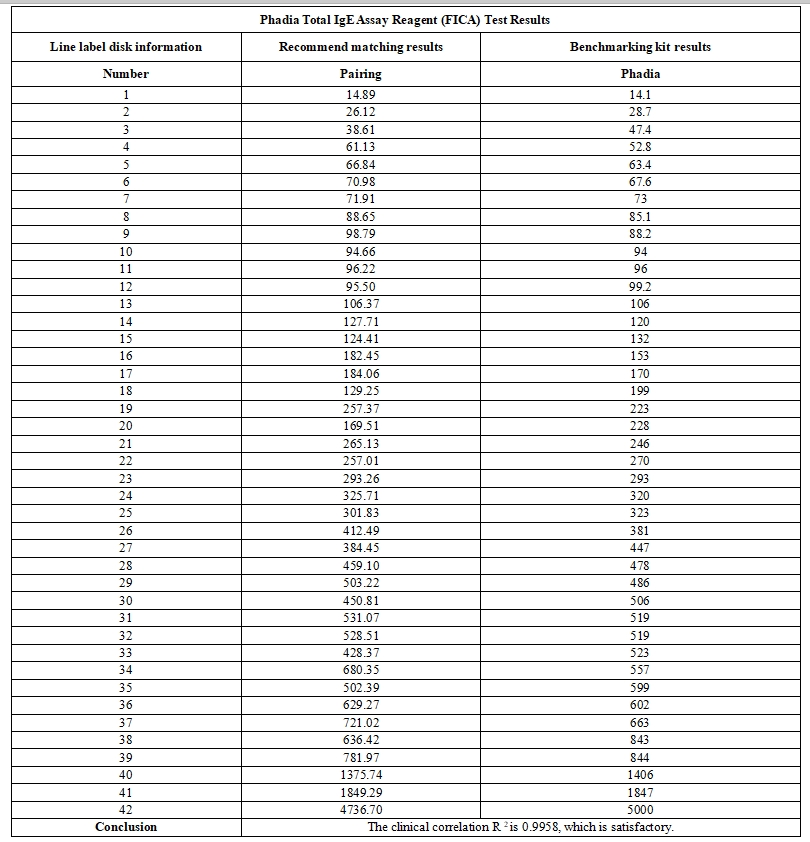
2. The comparison results of total IgE and industry benchmark kits are as follows:
3. Reagent performance results
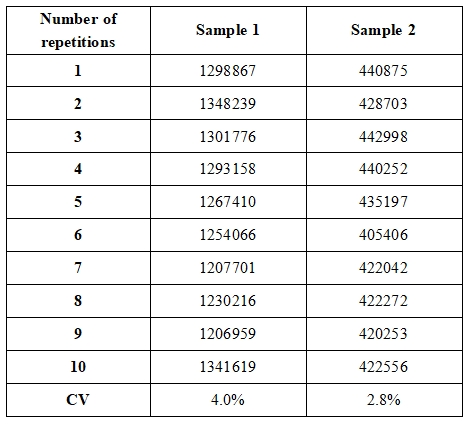
3.1 Repeatability
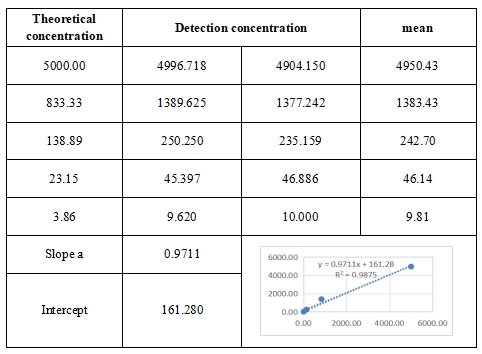
3.2 Linear range
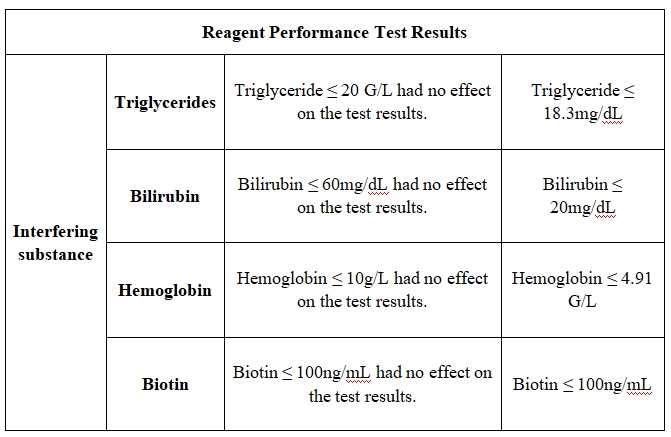
4. Anti-interference performance (sample concentration: 130 IU/mL and 325 IU/mL)
5. Stability of the reagent